Pupil reactivity, the eye’s ability to adjust its size in response to various stimuli, offers a unique window into brain function. By examining how pupils respond to light and other factors, health care professionals can gain valuable insights into the neurological status of an individual. This article delves into the mechanisms behind pupil reactivity, its significance in neurological assessments, and what different pupil responses can reveal about brain health.
Understanding Pupil Reactivity
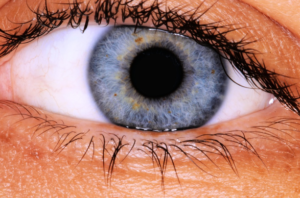
The pupil, the black circular opening in the center of the iris, regulates the amount of light entering the eye. Its size is controlled by two muscles:
- Sphincter Pupillae: A circular muscle that constricts the pupil in bright light conditions.
- Dilator Pupillae: A radial muscle that dilates the pupil in low light conditions.
These muscles are governed by the autonomic nervous system:
- Parasympathetic Nervous System: Stimulates the sphincter pupillae to constrict the pupil.
- Sympathetic Nervous System: Stimulates the dilator pupillae to dilate the pupil.
The balance between these systems ensures appropriate pupil size in response to varying light conditions and other stimuli.
The Pupillary Light Reflex
A key aspect of pupil reactivity is the pupillary light reflex, which involves the following pathway:
- Light Detection: Photoreceptors in the retina detect light and send signals via the optic nerve (cranial nerve II) to the brain.
- Signal Processing: These signals reach the pretectal nuclei in the midbrain.
- Bilateral Activation: The pretectal nuclei communicate with both Edinger-Westphal nuclei, leading to a bilateral response.
- Pupil Constriction: Parasympathetic fibers from the Edinger-Westphal nuclei travel with the oculomotor nerve (cranial nerve III) to innervate the sphincter pupillae muscles, causing pupil constriction.
This reflex ensures that both pupils constrict simultaneously when light is shone into one eye, a phenomenon known as the consensual response.
Neurological Insights from Pupil Measurements
Assessing pupil reactivity provides critical information about the integrity of neural pathways and brain function. Abnormal pupil responses can indicate various neurological conditions:
Relative Afferent Pupillary Defect (RAPD): Also known as Marcus Gunn pupil, RAPD is identified using the swinging flashlight test. In this test, a light is alternately shone into each eye. A positive RAPD is observed when the affected pupil dilates instead of constricting when the light is directed at it, suggesting optic nerve damage or severe retinal disease.
Third Nerve Palsy: Damage to the oculomotor nerve can lead to pupil dilation (mydriasis) and ptosis (drooping eyelid). The affected eye may also deviate outward and downward due to unopposed action of the lateral rectus and superior oblique muscles. Common causes include aneurysms, tumors, or increased intracranial pressure leading to uncal herniation.
Horner’s Syndrome: Characterized by a triad of ptosis (drooping eyelid), miosis (constricted pupil), and anhidrosis (lack of sweating) on the affected side. It results from disruption of the sympathetic pathways supplying the eye and can be caused by lesions anywhere along this pathway, including the hypothalamus, spinal cord, or sympathetic chain.
Adie’s Tonic Pupil: This condition presents as a dilated pupil with a sluggish or absent light response but a preserved or exaggerated response to near vision (accommodation). It is often idiopathic but can be associated with viral infections or trauma affecting the ciliary ganglion.
The Role of Pupil Reactivity in Assessing Brain Injuries
In emergency and critical care settings, pupil assessments are vital for evaluating patients with potential brain injuries. Changes in pupil size, shape, or reactivity can signal increased intracranial pressure (ICP), brain herniation, or brainstem dysfunction. For instance, bilateral fixed and dilated pupils may indicate severe brain injury or brain death.
Automated pupillometry devices have been developed to provide objective, quantitative measurements of pupil size and reactivity, reducing inter-examiner variability and improving the accuracy of neurological assessments.
Factors Influencing Pupil Reactivity
Several factors can affect pupil size and reactivity, including:
- Age: Pupil size generally decreases with age, and the speed of the pupillary light reflex may slow down.
- Medications: Certain drugs can cause pupil dilation (e.g., anticholinergics) or constriction (e.g., opioids).
- Lighting Conditions: Ambient light levels directly influence pupil size, with pupils constricting in bright light and dilating in darkness.
- Emotional State: Stress or arousal can activate the sympathetic nervous system, leading to pupil dilation.
- Fatigue: Tiredness can result in slower pupil reactions.
Conclusion
Pupil reactivity serves as a crucial indicator of neurological function, reflecting the complex interplay between various neural pathways. Regular assessment of pupil responses can aid in the early detection of neurological impairments, guide clinical decision-making, and monitor the progression of brain injuries.